Real-Time
In addition to the claims processing capabilities of ClaimConnect, DentalXChange also offers the ability to confirm patient eligibility, benefit details, and claim adjudication information from payers through the Real-Time package. Real-Time eligibility and benefits payers deliver up-to date information to DentalXChange regarding qualified patient information. This allows review of most patient eligibility and benefit information in real time.
Visit our Video Library for more helpful tutorials.
- Eligibility – a patient’s insurance plan status with the payer. Real-Time reports the status as either Active, Inactive, or Not Available.
- Benefits – a patient’s insurance plan coverage.
- Claim Status – the step that a claim has reached in the adjudication process.
- Note: Real-Time displays current information only as it is provided by the payer. Responses may vary dependent on the payer’s response level.
Confirming Payer Real-Time Participation
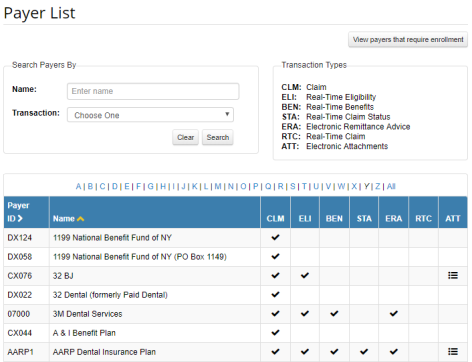
Providers can confirm which Real-Time Transactions are available for each payer by accessing the Payer List.
- After logging in and accessing Claim Connect, select thePayer List link in the left side menu.
- The Payer List displays.
- The Payer List details the transactions supported by each payer in a table format. Check marks indicate supported transactions.
- Note: Transactions that are not supported will result in less robust Real-Time responses.
- Enter a payer name in the Name field of the Search section to find a specific payer or,
- Enter a transaction type in the Transaction field of the Search section to find payers that support a specific transaction types.
- Review the Transaction Types section for the legend of available transaction types.
Eligibility & Benefits Search
|
|
Eligibility, Coverage or Benefit Inquiry ASC X12 270, also: 270 |
|
|
Eligibility, Coverage or Benefit Information ASC X12 271, also: 271 |
- Select the link below to view the video tutorial on this subject.
 How to Check Patients Eligibility
How to Check Patients Eligibility
- From the Dashboard page, under Electronic Claim Services, select the Eligibility button.
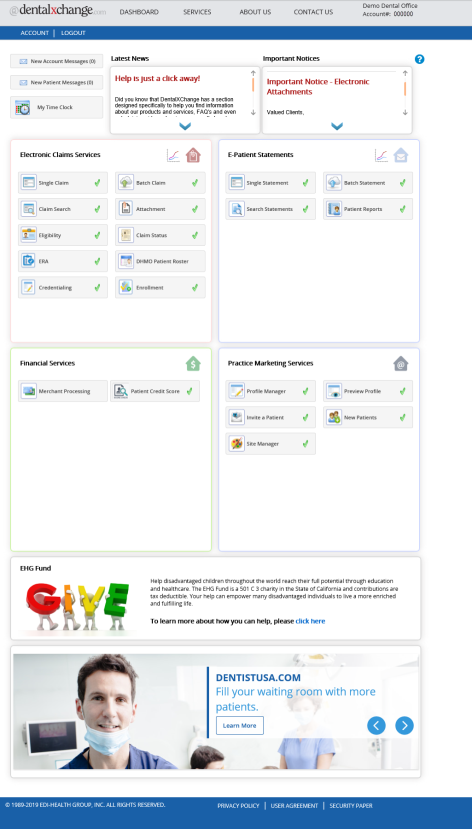
- Or, from the Welcome to ClaimConnect page, under Real-Time section of the menu, select the Eligibility link.
Eligibility Page
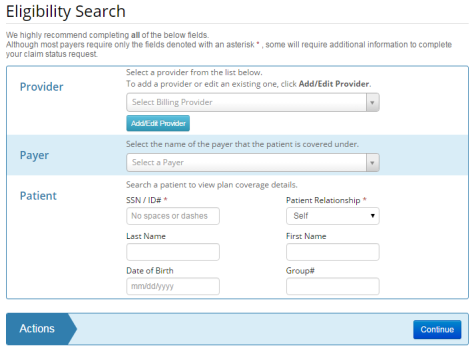
- Select or enter provider, patient, and payer information.
- Only Payers with supported eligibility and/or benefits transactions are selectable.
- Note: Fields not marked with an asterisk (*) may be required. Errors display for affected fields.
- Select Continue to proceed.
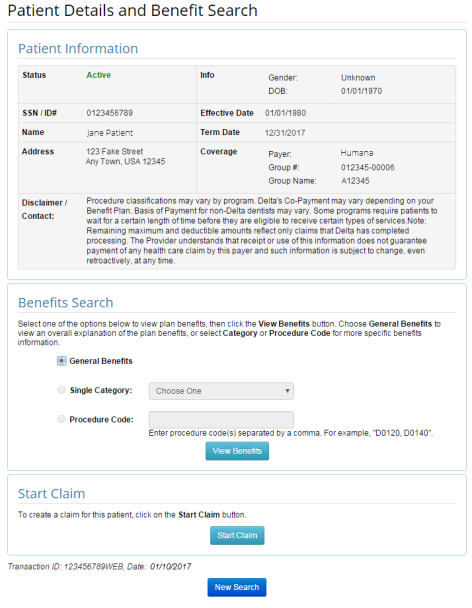
- The Patient Details and Benefit Search page displays.
- The Patient Details and Benefit Search page is a first response that provides general eligibility information.
- The patient’s current enrollment status displays in the Status field.
- Select the search criteria in the Benefits Search section to review more detailed benefits information where available.
- Select General Benefits to view an overall explanation of the plan benefits.
- Select Single Category or Procedure Code to narrow the results to a specific range of procedure codes or a single procedure code respectively.
- Select the View Benefits button to proceed.
- Note: Payers that support both Eligibility and Benefits transactions may provide more robust search results.
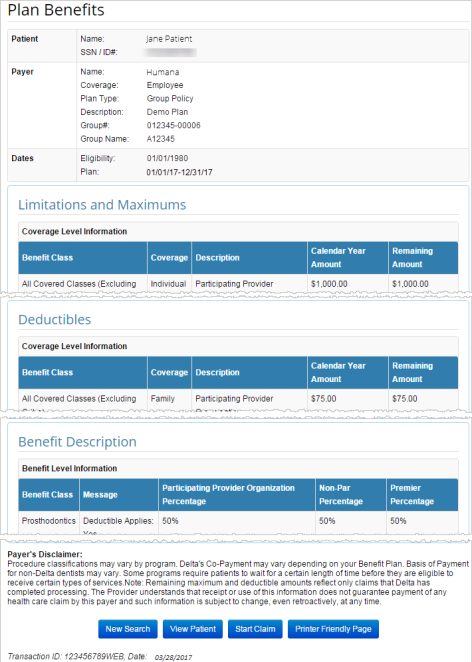
- The Plan Benefits page displays with patient benefits information where available.
- Additional actions are available at the bottom of the page:
- Select the View Patient button to return to the Patient Details and Benefits Search page.
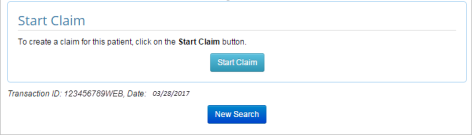
- Providers with a claim processing package, select Start Claim to submit a DDE Claim.
- Patient information from the Real-Time search is automatically populated in to the claim form.
- Providers with a claim processing package may also select Start Claim from the Patient Details and Benefits Search page to submit a DDE Claim.
- Select the New Search button to start a new Eligibility and Benefits search.
Claim Status
|
|
Health Care Claim Status Inquiry ASC X12 276, also: 276 |
|
|
Health Care Information Status Notification ASC X12 277, also: 277 |
Aside from providing access to patient eligibility information prior to providing service, Real-Time also grants the ability to review the status of a claim before it reaches its final outcome.
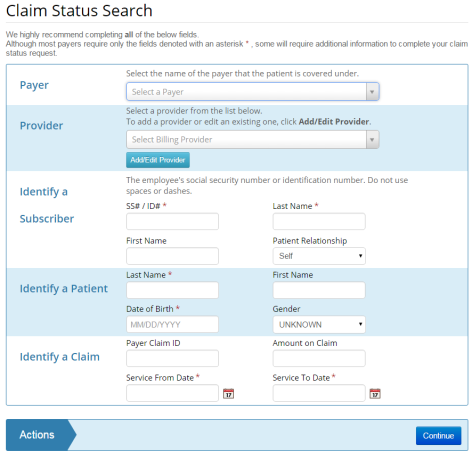
- From the Dashboard page, under Electronic Claims Services, select the Claim Status button, or
- From the ClaimConnect Welcome page select the Claim Status link in the Real-Time section of the menu.
- Select/Enter payer, provider, subscriber, patient, and claim information as necessary.
- Note: Fields not marked with an asterisk (*) may be required. Errors display for affected fields.
- Select Continue to proceed.
- The Claim Status Results page displays.
- Status, Claim Level Response, and Claim Item Response fields update as DentalXChange receives new information from the payer.
- Select the Update Status button to receive current information.
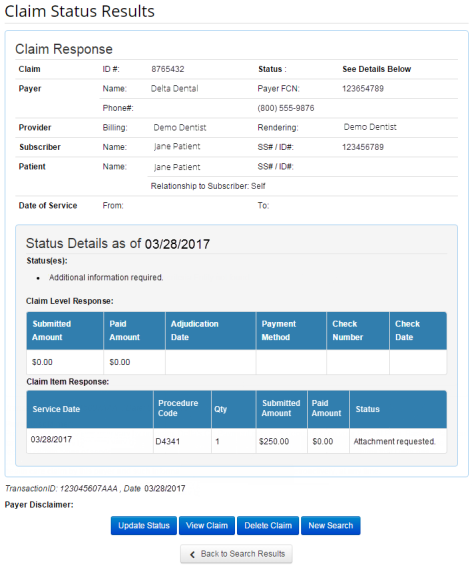
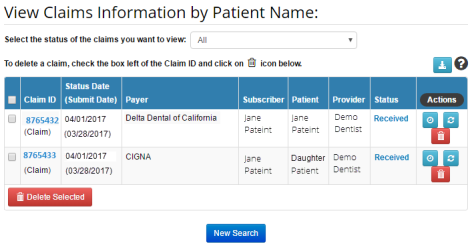
- Use the Advanced Search to review the status of several claims at once.
- Select the Refresh button
 to refresh the claim status.
to refresh the claim status.
Eligibility & Benefits with DMD
|
|
Eligibility, Coverage or Benefit Inquiry ASC X12 270, also: 270 |
|
|
Eligibility, Coverage or Benefit Information ASC X12 271, also: 271 |
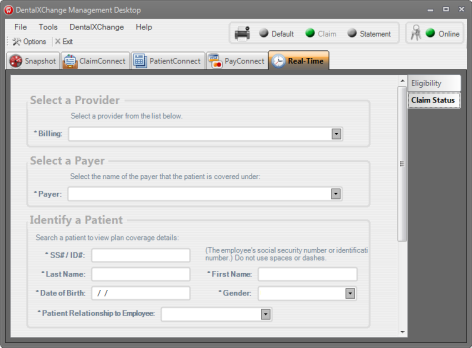
Providers who have downloaded and installed the DentalXChange Management Desktop (DMD) are also able to review eligibility and benefits information through the DMD without accessing the DentalXChange website directly.
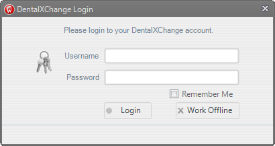
- Select the DMD Shortcut on the provider’s desktop to open DMD.
![]()
- Enter the DentalXChange account login information.
- Select the Login button to start the DMD.
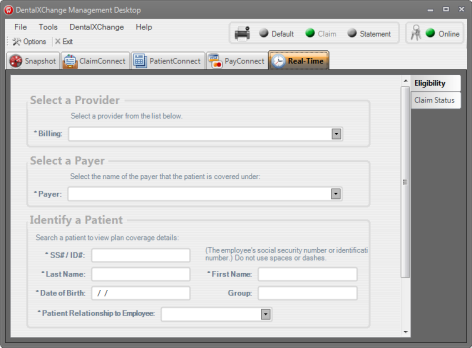
- Select the Real-Time tab in DMD.
- Confirm that the Eligibility tab is active.
- Enter the search criteria.
- Required fields are marked with an asterisk (*).
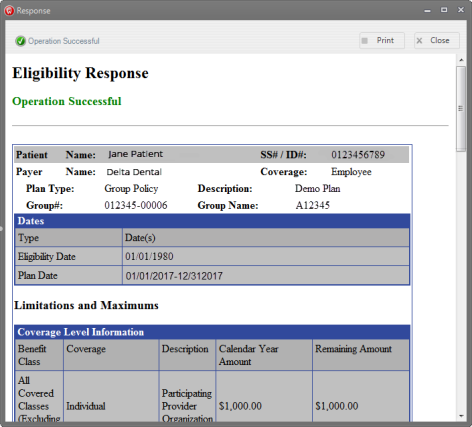
- The Eligibility Response displays in a separate window.
- Select the Print button to print a copy of the response.
- Select the Close button to close the window.
Claim Status with DMD
|
|
Health Care Claim Status Inquiry ASC X12 276, also: 276 |
|
|
Health Care Information Status Notification ASC X12 277, also: 277 |
Claim Status information is also viewable through DMD without accessing the DentalXChange website directly.
- Select the Real-Time tab in DMD.
- Confirm that the Claim Status tab is active.
- Enter the search criteria.
- Required fields are marked with an asterisk (*).
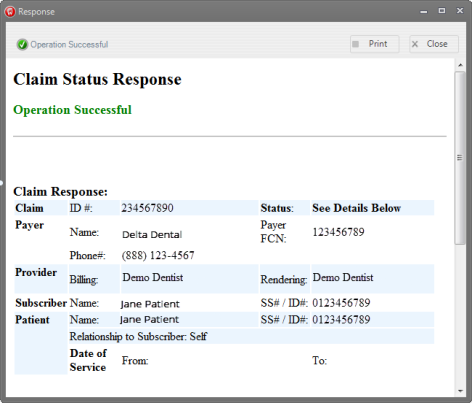
- The Claim Status Response displays in a separate window.
- Select the Print button to print a copy of the response.
- Select the Close button to close the window.
Software Integration
Providers with participating Practice Management Systems (PMS) can also complete Real-Time transactions using their PMS. Providers can review their PMS user guide for more information on setup. Eligible software includes:
- Denticon/Planet DDS
- Dentimax
- Dentisoft & Dentisoft Online
- Open Dental
- Practice Web
- The Digital Office (TDO)
*For further assistance, please Contact Us
