Electronic Remittance Advice
|
|
Health Care Claim Payment or Advice ASC X12 835, also: 835 |
An Electronic Remittance Advice (ERA) is an electronic document that is sent to a provider by an insurance payer detailing claim information pertaining to payment and the claim payment details with explanation. The ERA can also be described as the electronic version of the Explanation of Benefits (EOB) that a patient receives from the payer after the payer has processed the claim. Just like an EOB, an ERA provides information regarding the patient the service provider, and any adjustments made to the claim during processing. They also both include the type of procedure performed, when it was performed, and the cost. Additional information regarding the patient’s benefits is often included as well, including the details of the plan, such as co-payment and deductible information. If payment is denied an explanation is provided. As a software solution focused on EDI transactions, DentalXChange extends ERA services to providers with ClaimConnect services as a free enhancement to the account. Providers should contact DentalXChange support for more information on setting up their ClaimConnect account to receive ERAs.
Visit our Video Library for more helpful tutorials.
Summary Lists
ClaimConnect organizes ERAs into a series of lists to make it easy to visually identify payments that have been accounted for versus payments that have yet to be documented by the provider.
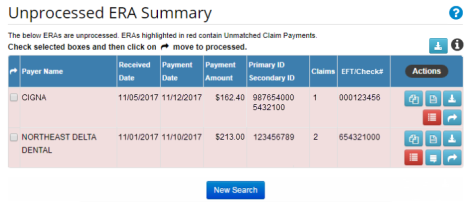
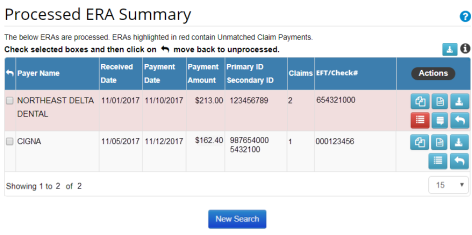
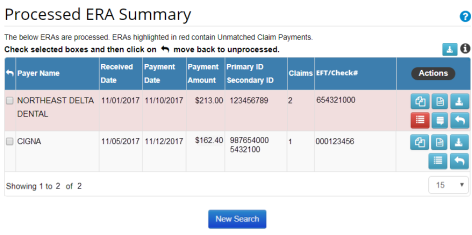
- During ERA searches ERAs display in a table format with several available actions and background colors.
- Items with a red background indicate that the report contains at least one unmatched claim payment, that is, a payment not matched to a claim.
- Items without a red background signify matched payments.
Reports
ERAs are submitted to DentalXChange as a block of reports. Each report may contain multiple claim payments for several different claims. Before a dental practice may receive ERA Reports the office needs to follow the enrollment process facilitated by DentalXChange for each insurance payer. The enrollment process varies by payer. Processing an ERA Report does not delete the report, it simply moves the report to the Previously Processed Reports category. Reports that have been processed can always be revered back to unprocessed.
- Note: Direct any questions about ERA enrollment to the DentalXChange Enrollment Department.
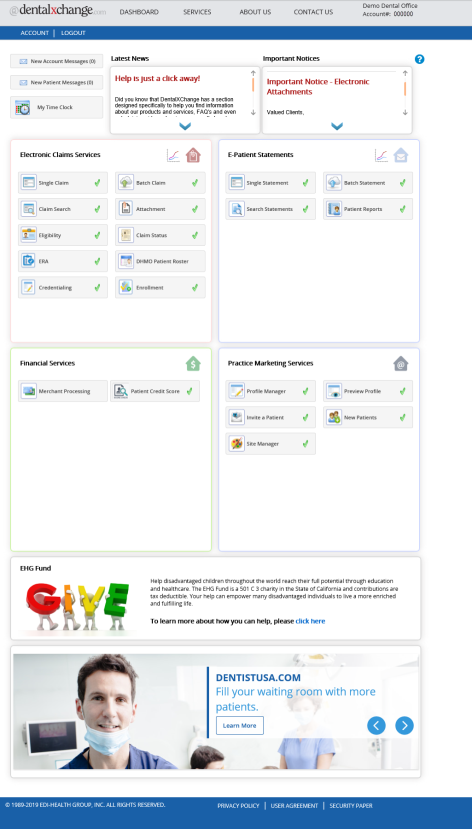
Locating ERA Reports
- To locate ERA Reports from the Dashboard page, select the Electronic Claim Services home
 button.
button. - Select the link below to view the video tutorial on this subject.
 Processing and Reviewing ERA Reports
Processing and Reviewing ERA Reports
- From the Welcome to ClaimConnect page, under Reports, select the ERA/Payments link.
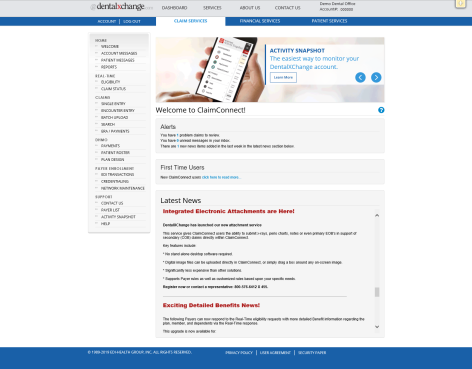 s
s
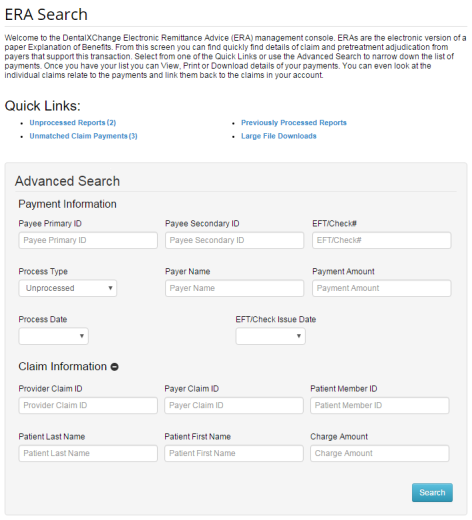
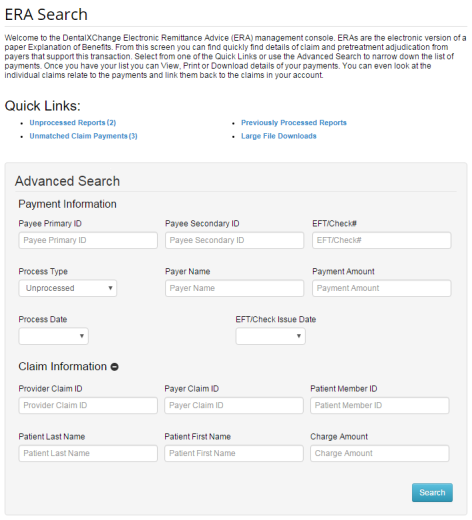
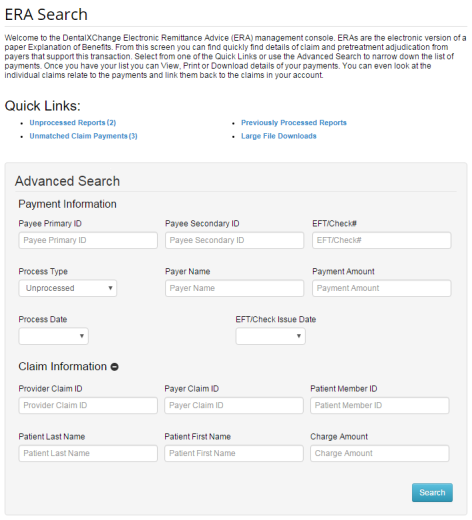
- The ERA Search Page displays.
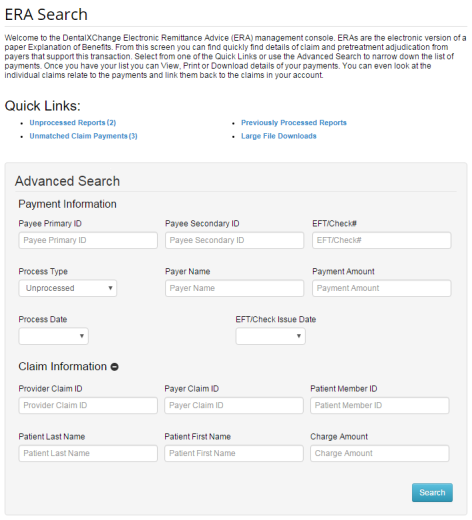
Searching for an ERA
- Under Quick Links select from the options of Unprocessed Reports, Unmatched Claim payments, Previously Processed Reports or Large File Downloads to view claim payment details.
- The Summary Page has a column of the available Actions that can be selected relative to each ERA on the list.
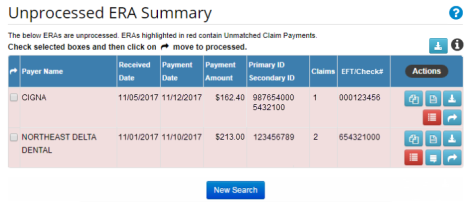
Download File
- Select the Download File
 button located above the table of search results as shown above to download an Excel version of the search results in Comma Separated Value (CSV) format.
button located above the table of search results as shown above to download an Excel version of the search results in Comma Separated Value (CSV) format.
Info
- Hover over the Info
 button for an explanation of the available Action buttons.
button for an explanation of the available Action buttons.
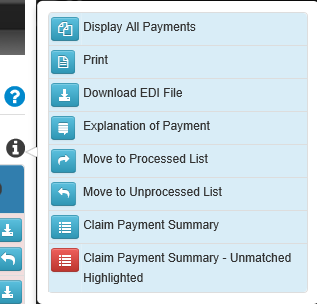
Display All Payments
- Select the Display All Payments
 button to review the selected ERA.
button to review the selected ERA.
- Select the Print
 button to print, save, and review a PDF version of the ERA.
button to print, save, and review a PDF version of the ERA. - ERA Print Option:
- Print with page break between claim payments: Each claim is printed on a page for easy filing with patient records;
- Add Claim Payment Summary: The Claim Payment Summary will be displayed; and,
- Save Settings.
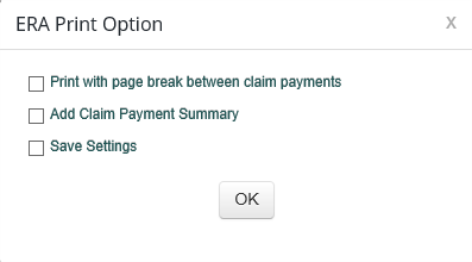
- Codes and descriptions listed for each claim are printed.
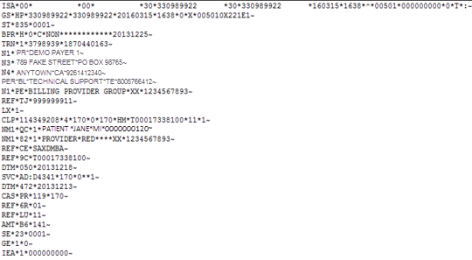
Download EDI File
- Select the Download EDI File
 button to download an EDI file (.835) for import in to a Practice Management System.
button to download an EDI file (.835) for import in to a Practice Management System. - Note: Certain Practice Management System (PMS) users may be restricted from downloading EDI files.
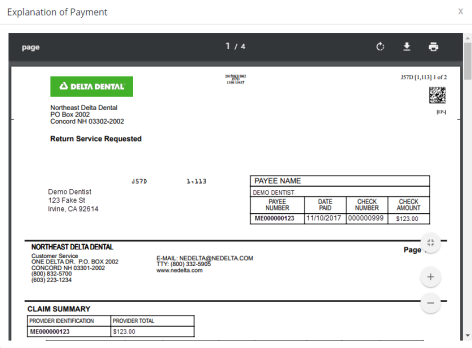
Explanation of Payment
- Select the Explanation of Payment
 button to view what normally would be received by mail.
button to view what normally would be received by mail. - Note: Not all payers support this functionality.
Move to Processed or Unprocessed List
- When all payments have been matched, select the Move to Processed List
 button to move an ERA to the Processed Payments List.
button to move an ERA to the Processed Payments List. - Note: To move multiple reports, in the left side column, select the check box next to the appropriate report, then the Move to Processed List button at the top of the column.
- The ability to move ERA reports to the Unprocessed List at any time is available by selecting the Move to Unprocessed List
 button.
button.
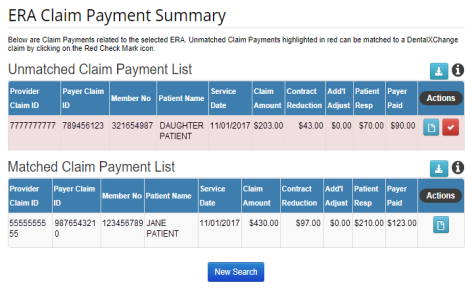
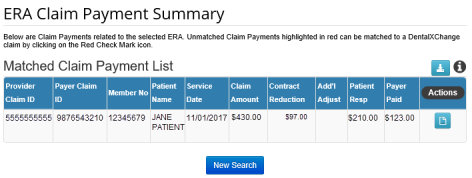
Claim Payment Summary
- Select the Claim Payment Summary
 button to view an ERA Claim Payment Summary.
button to view an ERA Claim Payment Summary. - The Claim Payment Summary page displays. Select the Display Claim Payment
 button to display the Electronic Remittance Advice – Notification Only which displays a list of the Claim information related to this payment.
button to display the Electronic Remittance Advice – Notification Only which displays a list of the Claim information related to this payment. - Payment may be filtered on only one claim. To view the full payment select the Display All Payments
 button.
button. - Note: Print and Download functions are available.
Advanced Search
The ERA Advanced Search allows a provider to search for an ERA with only a few pieces of information. ERAs can be found either with the payment information or with the claim information.
- Enter the search criteria into at least one of the blank fields, and select options from the drop-down menus where appropriate.
- Note: From the Process Type drop-down choose either Unprocessed Reports or Previously Processed Reports.
- At the bottom of the page select the Search button to view results.
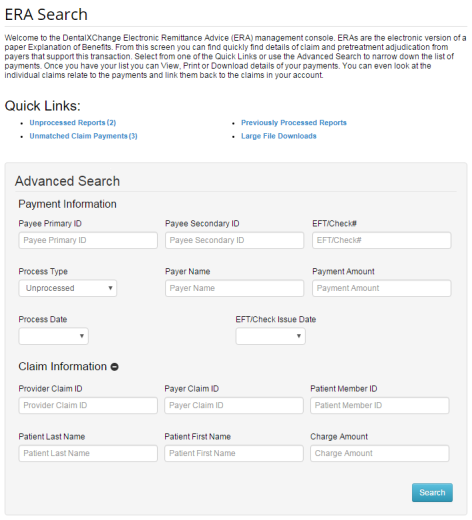
- The ERA Claim Payment Summary Page displays with a list of results that meet the search criteria. Select the New Search button to return to the ERA Search page.
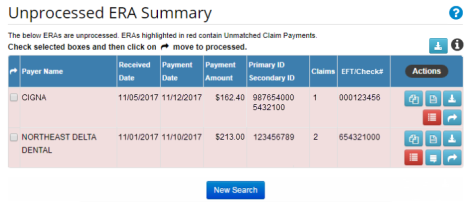
Unprocessed Reports
Unprocessed Reports are ERAs that have not been reviewed or processed manually by the provider. The Unprocessed Reports list can be used to separate ERAs that detail payments that have not been matched to a claim from ERAs that detail payments that have been matched to a claim. It is best practice to view and process reports in a timely manner in order to quickly address any issues and to keep this section organized. Reports may remain in the Unprocessed Reports section indefinitely.
- Select the Unprocessed Reports (#) link to view a list of unprocessed ERAs.
- The Unprocessed ERA Summary list displays.
- Select an Action to proceed.
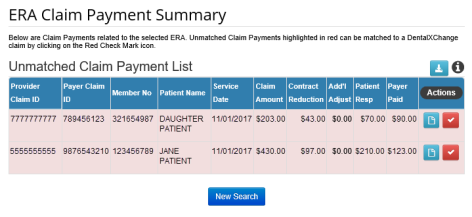
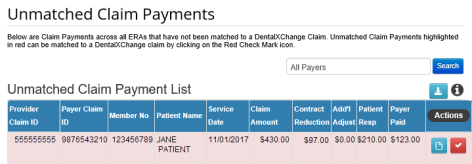
Unmatched Claim Payments
Unmatched Claim Payments are individual claim payments that have not been matched to their associated ClaimConnect claim. They include at least one payment that is unmatched to a DentalXChange claim. If at least one claim payment is unmatched the report will continue to appear as unmatched. Moving an ERA from Unprocessed to Processed will not change the match status. When moving an unmatched ERA into the Previously Processed Reports section the ERA report will continue to correctly show that it is unmatched.
- Select the Unmatched Claim Payments (#) link to view a list of unmatched payments.
- The Unmatched Claim Payments list displays a list of unmatched payments from unprocessed ERAs.
- To search and sort by payer enter a payer name in the All Payers text field and select the Search button to view results.
- Select an Action to proceed.
- To view an ERA select the Display Claim Payment
 button.
button.
Matching a Claim to a Claim Payment
- To match a payment to a claim select the Match Claim Payment to Claim
 button.
button. - The Match Claim Payment screen displays in a pop up window.
- The right side displays claim payment details from the ERA.
- ClaimConnect automatically attempts to locate the matching claim based on the information contained in the ERA.
- The left side allows for searching for a matching claim by Patient Last Name, Subscriber ID, Provider Claim ID or any combination of these options when ClaimConnect is unable to automatically locate a claim.
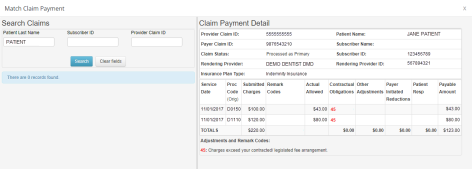
- Select the Search button to locate the claim.
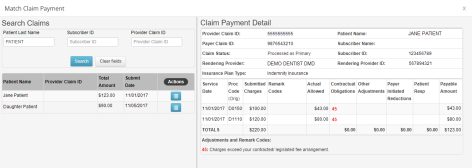
- Available search results appear.
- Select the Display Claim
 button for the claim to be matched to the payment.
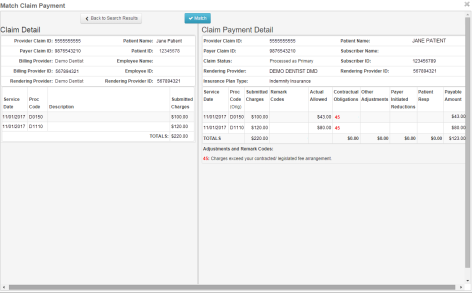
button for the claim to be matched to the payment. - Confirm that the claim details on the left match the payment details on the right.
- Select the Match button to match the claim to the claim payment.
- The claim payment is no longer listed as unmatched.
- A single ERA report may contain many payments for several different claims. If at least one claim payment is unmatched the report will continue to appear unmatched.
- After completing the match process, the ERA Claim Payment Summary page displays showing that the newly matched payment has moved to the Matched Claim Payment list.
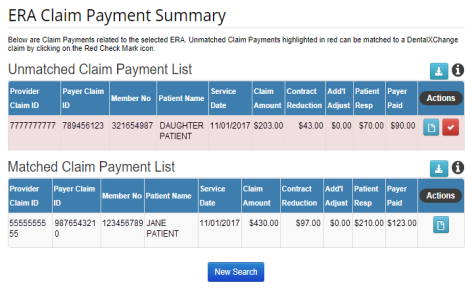
- Return to the Unprocessed Reports list to move the ERA from the Unprocessed ERA Summary list to the Processed ERA Summary list. Any additional unmatched payments within the ERA report will remain unmatched.
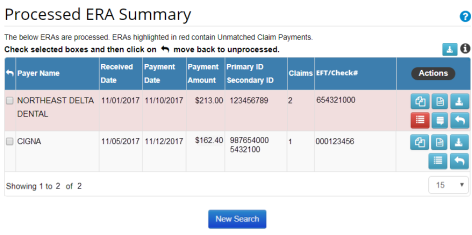
Previously Processed Reports
Previously Processed Reports are ERAs that have been reviewed or marked as processed by the provider. The Previously Processed Reports list can be used to separate ERAs that detail payments that have been matched to a claim from ERAs that detail payments that have not been matched to a claim.
- Select the Previously Processed Reports link to view a list of processed ERAs.
- The Processed ERA Summary page displays the list of ERAs that have been marked as processed.
- Refer to Searching for an ERA for further details on the actions available.
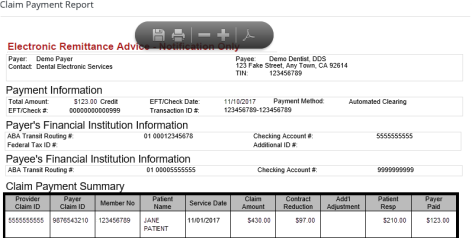
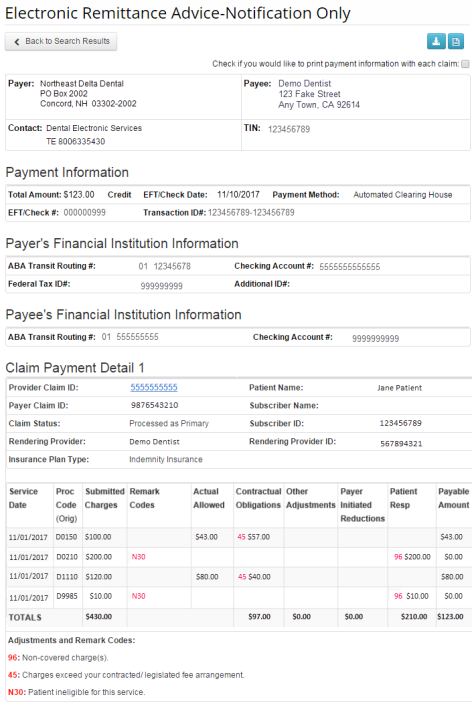
Reading an ERA
Insurance payers determine the format of an ERA so each may look slightly different. The ERA displayed below has the following sections:
- Payer and Payee information:
- The top portion of the ERA lists the basic contact information for both the payer who processed the claim, and the provider who submitted the claim.
- Payment and Financial Institution information:
- The Payment and Financial Institution information sections detail all the information involved in any payments made. This information includes payment amounts, payment dates, and payment method.
- Note: The Payment information section of the ERA simply provides information on the payment that has been made and does not detail amounts paid toward multiple claims within the same lump payment.
- Claim Payment Detail information:
- The Claim Payment Detail information section is where the breakdown of amounts paid is detailed.
- This section also details any claim payment adjustments, payment amounts to be paid by the patient, and any additional remarks on the amounts paid.
*For further assistance, please Contact Us
