Dental Health Maintenance Organization
Online Dental Health Maintenance Organization Services are part of DentalXChange ClaimConnect. Claims submitted for subscribers who are part of a special network of dental professionals, known as a Dental Health Maintenance Organization (DHMO), use a different kind of claim. Dental Health Maintenance Organizations are insurance plans that restrict the subscriber to services rendered only from network dental professionals. For submitters, DHMOs provide a fixed payment on a regular basis, usually monthly, regardless of how many patients they see. A claim submitted to a DHMO insurance company is called an Encounter. The Practice must first sign up for the Online DHMO Services package.
Visit our Video Library for more helpful tutorials.
Aetna DHMO
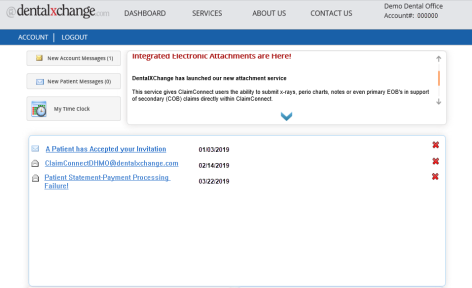
- To check a practice has signed up for the Package Online DHMO Services Package, select Account from the dashboard page.
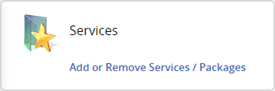
- From the Account page, under the Services section, select Add or Remove Services / Packages.
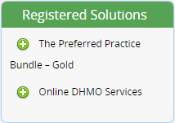
- Ensure Online DHMO Services are appearing under Registered Solutions.
- Add the Online DHMO Services if it is not appearing.
- Select Account.
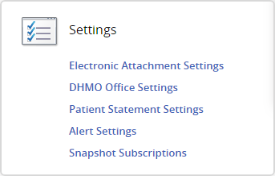
- Select under settings DHMO Office Settings.
- Enter the Aetna Office ID or enter the Group Health Cooperative of South Central Wisconsin ID.
- If office doesn’t have the Aetna ID, the practice will need to call Aetna at (800)-451-7715 or check the ID in Aetna DocFind.
- Select the Save button.
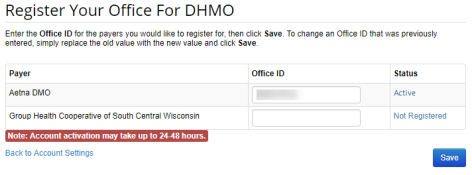
- Account activation may take 24 to 48 hours for DentalXChange to verify the ID.
- DentalXChange will send the confirmation email to practice once completed.
- Allow 10-14 business days to start receiving Roster online.
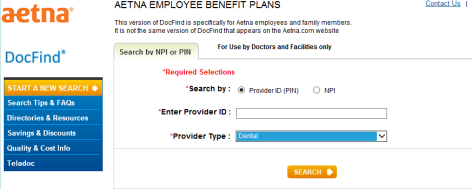
Find A Provider ID on Aetna website
- Navigate to Aetna's website.
- Select tab labeled Search by NPI or PIN.
- Select Provider ID (PIN) in Search by field.
- Enter Provider ID.
- Select Dental in Provider Type field.
- Make sure the Aetna address matches DentalXChange’s provider address in DentalXChange account.
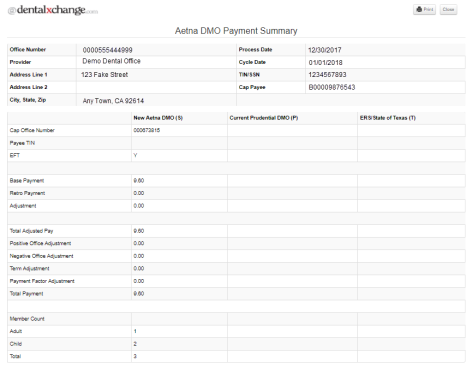
Payments
DHMO Payment report can be generated by DentalXChange including capitation payments, monthly active patient rosters and co-payment information and monthly terminated patient rosters. Follow below instructions to generate reports on the DentalXChange website.
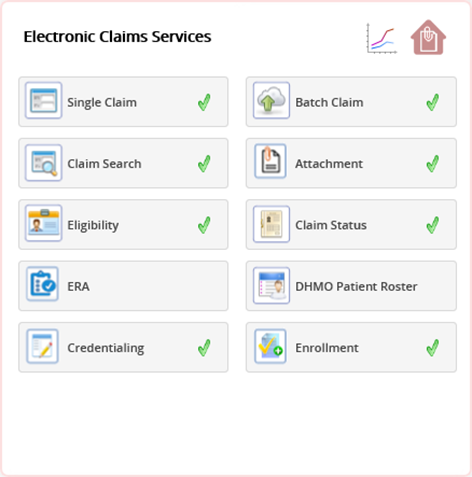
- Select ClaimConnect Home icon from Dashboard page under Electronic Claims Services.
- Under the DHMO section, select the Payments link.
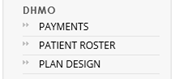
- Select Payer from drop-down.
- There are 2 different reports to choose from.
- Capitation Payments
- Monthly Active Patient Roster with Copayment Information
- Select desired report type from drop down list.
- Select View button to open report in a separate window.
- Select Download button to download report to computer in excel spreadsheet.
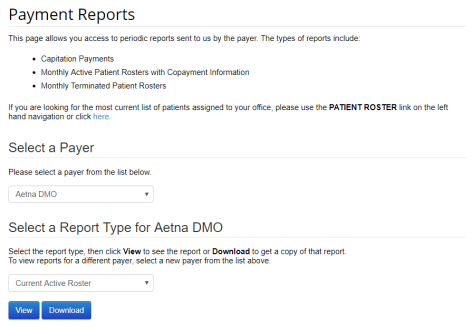
- Report: Current Active Roster.
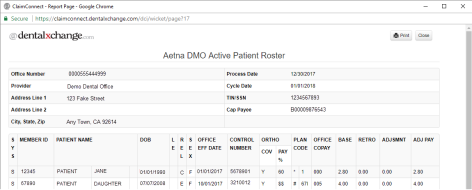
- Report: Payment Summary.
- The report will display a breakdown of the monthly Aetna payments including any adjustments and terminations.
Patient Roster
- Select Patient Roster under the DHMO section of the ClaimConnect home page.
- Select Payer from drop down.
- Select Plan from drop down.
- Select View to open report in a separate window.
- Select Download to download report to computer in excel spreadsheet.
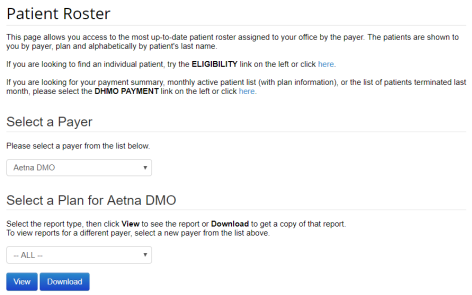
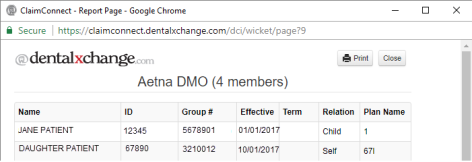
- Patient Roster Report.
- Note: Patient Roster Reports show all previous and current DHMO patients for the provider.
- Note: A date listed in the Term column reflects the termination date for inactive patients.
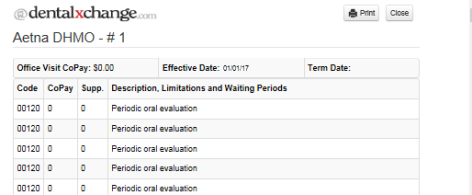
Plan Design
- Plan Designs report is also available listing copay amounts associated with covered procedures.
- Select Plan Design under the DHMO section of the ClaimConnect home page.
- Select Payer from drop down.
- Select Plan from drop down.
- Select View to open report in a separate window.
- Select Download to download report to computer in excel spreadsheet.
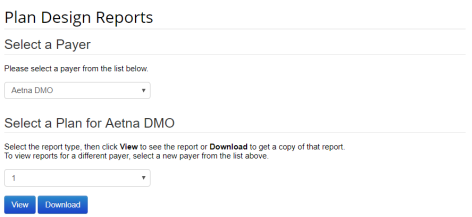
- Plan Design Report.
*For further assistance, please Contact Us